
Making a decision about Airway Clearance Techniques in Bronchiectasis
Discover airway clearance techniques tailored to your needs, empowering you to breathe easier and improve your quality of life through proven methods.
What is this website for?
This web page has been created to help you make a decision, it is often referred to as a decision aid or shared decision making tool. It is for people who have been told they have bronchiectasis. It will help you decide between the different airway clearance techniques (sometimes called breathing exercises) available to help manage your symptoms.
You should read all sections before your next appointment with your specialist, physiotherapist or bronchiectasis team to help you make a decision on the best airway clearance technique for you.
What is bronchiectasis?
Find out what causes bronchiectasis, how it affects your lungs, and why managing mucus buildup is so important. Read more
What are my airway clearance technique choices?
Compare the most commonly used airway clearance methods and see which one might suit your lifestyle best. Read more
What are airway clearance techniques?
Get a quick overview of how airway clearance techniques help you manage bronchiectasis more effectively. Read more
Questionnaire
Discover how a conversation with your physiotherapist can guide you to the right technique. Read more
Why are airway clearance technique important?
See how these techniques can reduce symptoms, prevent infections, and give you more control over your health. Read more
What is bronchiectasis?
Bronchiectasis is a long term condition affecting the airways in the lungs. The airways have become damaged and widened due to inflammation and can develop ‘pockets’ due to some scarring and weakness in the airways. These ‘pockets’ in the airways mean that mucus (sometimes called phlegm or sputum) gets trapped. The trapped mucus doesn’t get removed as quickly as usual and this allows bugs that land in the lung to stay down in the lungs. Once the bugs grow to a certain level a chest infection or flare up occurs.
Airway changes during a flare up in bronchiectasis can cause symptoms such as an increase in cough and mucus production, feeling more out of breath compared to your normal, generalised aches, chest discomfort and feeling more tired.

What are airway clearance techniques?
Airway clearance techniques (ACTs), sometimes called “breathing exercises” help to loosen mucus caught in the ‘pockets’ in your airways. ACTs move mucus from the smaller airways (deep inside your lungs) to the larger airways (towards the middle of your chest) up to the throat to be coughed or huffed out.
Why are they important?
Airway clearance techniques reduce symptoms such as excessive coughing. Most people cough to clear the mucus, but coughing alone is not enough to move mucus from the deeper airways inside your lung. People who perform regular airway clearance techniques have less day to day symptoms from their bronchiectasis.
Airway clearance techniques help reduce your risk of future chest infections. Some people with bronchiectasis do not produce much mucus but will still benefit from using ACTs for when they have more mucus symptoms, for example during a chest infection. Performing regular ACTs helps you take control of your health.
In the UK 70 in every 100 patients who have bronchiectasis use an airway clearance technique. Some people may choose not to perform airway clearance; however, it is recommended that all patients with bronchiectasis use an airway clearance technique.
What are my airway clearance technique choices?
There are many different ACTs available. When making this decision aid, we spoke with patients living with bronchiectasis and specialist bronchiectasis physiotherapists from around the United Kingdom (UK). We found that the three ACTs listed here were voiced as the most appropriate ones to initially offer patients with bronchiectasis.
Please click on each section to learn more.
Active Cycle of Breathing Technique
The Active Cycle of Breathing Techniques (ACBT) is one way to help you to clear mucus from your chest. ACBT is a set of breathing exercises that loosens and moves the mucus from your airways.
The Active Cycle of Breathing Techniques (ACBT) is one way to help you to clear mucus from your chest. ACBT is a set of breathing exercises that loosens and moves the mucus from your airways.
The ACBT combines different breathing techniques that help clear mucus from the lungs in three phases. The first phase, called “breathing control” helps you to relax and control your breathing. This also helps relax your airways. The second phase, called “deep breathing” helps to get air behind trapped mucus. The third phase, called “huffing” helps force the mucus out of your lungs. These three phases are performed in a cycle, sometimes more than once.


In the UK 51 in every 100 patients who perform an airway clearance technique, perform the ACBT
Autogenic Drainage
Autogenic drainage (AD) is an ACT which uses controlled breathing with different amounts of air in the lungs (different lung volumes) to unstick, collect and move mucus in three stages towards the top of your lungs.
Mucus which is lower down in the airways is moved by using a small amount of air in your lungs (breathing at low lung volumes). Whereas mucus in the top of your lungs is moved and cleared by using a larger amount of air in your lungs (breathing at higher lung volumes).

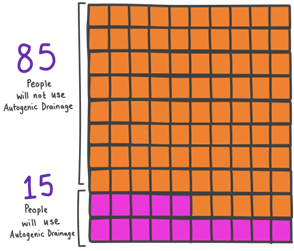
In the UK 15 in every 100 patients who perform an airway clearance technique, perform Autogenic Drainage
Oscillating Positive Expiratory Pressure (OPEP) Devices
Oscillating Positive Expiratory Pressure (OPEP) devices cause the air travelling from your lungs to vibrate (oscillate), which help loosen mucus from the airway walls.
These devices also provide a slight positive pressure as you breathe out through them. This positive pressure in your airways help them to stay fully open rather than closing down early when you breathe out, which can occur in some patients with bronchiectasis. Keeping the airways more open helps move mucus. This then helps move the mucus from the smaller airways deeper in your lungs, to the larger airways near the top of your lungs for removal.

This is a list of common OPEP devices available in the UK. Which device you will be offered will depend on what is available in your area:
| Acapella | ICU Medical |
| Aerobika | Trudell Medical International |
| Flutter | Clement Clarke International |
| Lung Flute | Medical Acoustics LLC |
| RC Cornet | Henleys Medical Supplies |
Devices are listed in alphabetical order


In the UK 24 in every 100 patients who perform an airway clearance technique, use an OPEP device
Tailored Guidance for Choosing Airway Clearance Methods
There are different types of ACTs. What matters to you is an important part of making a decision about treatment. Please fill out the following form. Your answers will be shared with your physiotherapist.
This form has 4 parts and will take approximately 5 minutes to complete.
You will go through 4 parts and then submit.
This table describes some facts about the three options. There are very few studies that compared the same type of facts for each option. Most of these studies involved speaking to patients with bronchiectasis and respiratory physiotherapists, rather than a scientific test.
| Advantages | Active Cycle of Breathing Technique (ACBT) | Autogenic Drainage (AD) | Oscillating Positive Expiratory Pressure (OPEP) |
| You can perform independently | ✔️ | ✔️ | ✔️ |
| You can perform it anywhere | ✔️ | ✔️ | ✔️ |
| You have to clean equipment or device regularly | ✖️ | ✖️ | ✔️ |
| You have to replace equipment or device (usually every 6-12 months) | ✖️ | ✖️ | ✔️ |
| Provides a visual or physical prompt to remind you to perform it | ✖️ | ✖️ | ✔️ |
| Cost associated with equipment or device | ✖️ | ✖️ | ✔️ |
| Can move mucus in specific parts of the lung | ✖️ | ✔️ | ✖️ |
| Can be used with nebuliser treatments | ✔️ | ✖️ | ✔️ |
| Disadvantages | |||
| Can be a difficult technique to understand and / or perform | ✔️ | ✔️ | ✖️ |
| It can take longer to perform than other techniques | ✖️ | ✔️ | ✖️ |
| Rarely people have had minor haemoptysis (coughing up a small amount of blood | ✖️ | ✖️ | ✔️ |
| Can be difficult to open, close or adjust equipment or device | ✖️ | ✖️ | ✔️ |
(Burnham, B., Stanford, G., and Stewart R. 2021), (Chaudary, N. and Balasa, G. 2021), (Herrero-Cortina, et al. 2023), (Kim, et al. 2023)
What else can I do to help my lungs?
Regular movement and physical activity are important for your lungs. They increase the strength of your muscles around your lungs and the rest of your body. This means you will be able to breathe more easily when you are active. Being active can also help you sleep better and improve your mental health and wellbeing. There are also alternative activities that may support your breathing such as singing and playing musical instruments. There is more information on how to keep active and alternative activities for your lungs on the websites below. If you would like a printed copy, please ask your respiratory physiotherapist.


Where can I find additional information on ACTs and bronchiectasis?
1. Asthma and Lung UK: https://www.asthmaandlung.org.uk/conditions/bronchiectasis
2. Living your life with Bronchiectasis:
https://www.bronchiectasis.me
3. The Bronchiectasis Toolbox:
https://bronchiectasis.com.au
Sources of Information
1. Burnham, P., Stanford, G. and Stewart, R., 2021. Autogenic drainage for airway clearance in cystic fibrosis. Cochrane Database of Systematic Reviews, (12).
2. Chaudary, N. and Balasa, G., 2021. Airway clearance therapy in cystic fibrosis patients insights from a clinician providing cystic fibrosis care. International journal of general medicine, pp.2513-2521.
3. Herrero-Cortina, B., Lee, A.L., Oliveira, A., O’Neill, B., Jácome, C., Dal Corso, S., Poncin, W., Muñoz, G., Inal-Ince, D., Alcaraz-Serrano, V. and Reychler, G., 2023. European Respiratory Society statement on airway clearance techniques in adults with bronchiectasis. European Respiratory Journal, 62(1).
4. Kim, S.R., Kim, S.H., Kim, G.H., Cho, J.Y., Choi, H., Lee, H., Ra, S.W., Lee, K.M., Choe, K.H., Oh, Y.M. and Shin, Y.M., 2023. Effectiveness of the use of an oscillating positive expiratory pressure device in bronchiectasis with frequent exacerbations: a singlearm pilot study. Frontiers in Medicine, 10, p.1159227.
5. Spinou, A., Hererro-Cortina, B., Aliberti, S., Goeminne, P.C., Polverino, E., Dimakou, K., Haworth, C.S., Loebinger, M.R., De Soyza, A., Vendrell, M. and Burgel, P.R., 2024. Airway clearance management in people with bronchiectasis: data from the European Bronchiectasis Registry (EMBARC). European Respiratory Journal, 63(6).
If you wish to use this patient decision aid for research, please contact Paul McCallion about collaboration.
Paul McCallion (p.mccallion2@newcastle.ac.uk) – Newcastle University and Newcastle Upon Tyne Hospitals NHS Foundation Trust, UK.